-
PDF
- Split View
-
Views
-
Cite
Cite
Moritz Wagner, Craig Butler, Matthias Rief, Mark Beling, Tahir Durmus, Alexander Huppertz, Antje Voigt, Gert Baumann, Bernd Hamm, Alexander Lembcke, Thomas Vogtmann, Comparison of non-gated vs. electrocardiogram-gated 64-detector-row computed tomography for integrated electroanatomic mapping in patients undergoing pulmonary vein isolation, EP Europace, Volume 12, Issue 8, August 2010, Pages 1090–1097, https://doi.org/10.1093/europace/euq135
Close - Share Icon Share
Abstract
To compare non-gated vs. electrocardiogram (ECG)-gated 64-detector-row computed tomography (MDCT) of the left atrium (LA) for integrated electroanatomic mapping (EAM) in patients with paroxysmal atrial fibrillation (AF).
Twenty-nine consecutive patients with paroxysmal AF underwent MDCT prior to pulmonary vein isolation (PVI). All patients were in sinus rhythm both during CT imaging and PVI. Multi-detector-row computed tomography was performed in 15 patients without ECG-gating (non-gated MDCT) and in 14 patients with retrospective ECG-gating (ECG-gated MDCT). Image quality of LA reconstructions from MDCT was rated on a five-point scale (from 1 = excellent to 5 = segmentation failed). Registration error between LA geometry obtained from EAM and MDCT was calculated as the mean distance between EAM points and MDCT surface. In all patients, LA was successfully segmented from MDCT data. The segmentation process took 2:31 ± 0:54 min for non-gated MDCT and 2:36 ± 0:47 min for ECG-gated MDCT ( P = 0.8). Image quality scores of LA reconstructions from non-gated and ECG-gated MDCT were 1.3 ± 0.6 and 1.4 ± 0.7, respectively ( P = 0.76). There was no significant difference in the registration error between non-gated and ECG-gated MDCT (1.8 ± 0.2 vs. 1.9 ± 0.3 mm, respectively; P = 0.6). The radiation dose of non-gated MDCT was significantly lower compared with ECG-gated MDCT (4.6 ± 1.4 vs. 13.4 ± 3.6 mSv, respectively; P < 0.001).
Non-gated MDCT depicts LA with appropriate image quality for integrated EAM, while exposing patients to substantially lower radiation dose compared with ECG-gated MDCT.
Introduction
Atrial fibrillation (AF) affects up to 5% of adults over 65 years of age and is understood to be triggered by focal electrical impulses from the pulmonary veins (PVs). 1 Electrical isolation of the PVs (PVI) through catheter-based delivery of radiofrequency energy has emerged as an effective and often curative therapy for patients with refractory AF. 2 Non-invasive imaging of the left atrium (LA) and PVs prior to PVI has become commonplace within the electrophysiology community. 2–7 In particular, multi-detector-row computed tomography (MDCT) is frequently used for integration of three-dimensional reconstructions of LA into electroanatomic mapping (EAM) systems to guide catheter ablation. Multi-detector-row computed tomography can thereby be performed with or without retrospective electrocardiogram (ECG)-gating, in which ECG-gated MDCT exposes patients to higher radiation doses due to the acquisition of highly overlapping slices. 4 , 8 In spite of relatively high radiation exposure, retrospectively ECG-gated MDCT is the method of choice for many centres, especially when patients are in sinus rhythm and LA reconstructions are used for integrated EAM. 5 , 9–14
The decision to use ECG-gated MDCT prior to PVI and its concomitant radiation exposure is problematic for two reasons: (i) patients undergoing PVI will receive a significant additional effective radiation dose from procedural fluoroscopy of 15–20 mSv 15–17 and (ii) it is currently recommended to have a low threshold for performing post-procedural follow-up imaging studies that intuitively should employ the same imaging technique used pre-procedurally. 2 Thus, there is a need for reduction of radiation dose of pre-procedural CT imaging. We hypothesize that imaging of LA with 64-detector-row CT can be performed without ECG-gating and will still provide sufficient image quality for integrated EAM, while exposing the patient to a significantly lower radiation dose compared with ECG-gated MDCT.
Methods
Patients
This retrospectively designed study was approved by the local Ethics Committee. The study population consisted of 29 consecutive patients with paroxysmal AF who underwent PVI with integrated EAM. Three patients had concomitant coronary artery disease. We included only patients with sinus rhythm during both CT imaging and PVI. Pre-procedural CT imaging was performed in 15 patients [mean age 60 years (range 39–79 years), 8 women, 7 men] with non-gated MDCT, whereas 14 patients [mean age 61 years (range 41–72 years), 9 women, 5 men] underwent ECG-gated MDCT prior to PVI. Six patients had a pacemaker implanted, in which two patients underwent ECG-gated MDCT and four patients underwent non-gated MDCT. The mean short-axis diameter of the LA defined by echocardiography in patients undergoing non-gated and ECG-gated MDCT was 41 ± 7 mm (range 27–51 mm) and 43 ± 7 mm (range 28–58 mm), respectively. Patients of both groups were comparable with regard to heart rate and body weight.
Computed tomography
All patients were examined using a 64-detector-row CT scanner with a gantry rotation time of 330 ms (Sensation 64, Siemens Healthcare, Erlangen, Germany). Non-gated MDCT was performed after intravenous injection of 80 mL contrast agent (Iopromid, Ultravist ® 370, Bayer Schering Pharma, Berlin, Germany) into the cubital vein at an infusion rate of 5 mL/s with the following acquisition parameters: tube voltage 120 kV, pitch 1.0, collimation 64 × 0.6 mm, and reconstructed slice thickness 0.75 mm. Electrocardiogram-gated MDCT was performed after intravenous injection of 80–120 mL contrast agent (Iopromid, Ultravist ® 370, Bayer Schering Pharma) at an infusion rate of 5 mL/s with the following acquisition parameters: tube voltage 120 kV, pitch 0.2, collimation 64 × 0.6 mm, reconstructed slice thickness 0.75 mm, and ECG-dependent tube current modulation as described previously. 18 Both ECG-gated and non-gated MDCT were performed with anatomically adapted tube current modulation based on attenuation profiles in the anteroposterior and lateral directions. 18
Image segmentation
Segmentation of MDCT data sets was performed using the semi-automated image integration software of an EAM system (CartoMerge™ Image Integration Module, Biosense Webster, Inc., Diamond Bar, CA, USA). Segmentation was performed by one cardiologist (T.V.) blinded as to whether the images were acquired using ECG-gated or non-gated MDCT. Image segmentation refers to the semi-automatic separation of individual cardiac structures from the MDCT data sets. 12 A manual editing tool was also used to optimize the LA reconstruction and to truncate PVs 3–4 cm distal to the PV ostium.
Electroanatomic mapping and fusion of computed tomography images with electroanatomic mapping data
Quadripolar electrophysiological diagnostic catheters were placed via a transfemoral approach in the distal coronary sinus and at the position of the His-potential. With these as anatomical landmarks, two standard pressure-controlled transseptal punctures were performed, and a steerable 8.5 F and a non-steerable 8.0 F transseptal sheaths were placed into the LA. Thereafter, EAM was performed with a 3.5 mm irrigated-tip catheter (NaviStar ThermoCool, Biosense Webster), taking contact points equally distributed over the body of the LA. Electroanatomic mapping of PVs was performed by manoeuvring the catheter 3–4 cm into each PV and slowly pulling it back to the LA. Therefore, final EAM data included mapping points of PVs and the body of the LA. Internal points were deleted. After manual adaptation of EAM data with the CT image, a landmark point was selected at the central posterior LA wall as the anchor point for fusion. Surface alignment of the body of the LA and the PVs was optimized by an automatic algorithm as described previously. 19
Image quality and accuracy of left atrial reconstruction
Image quality of LA reconstructions was assessed by two readers (T.V. and M.W.) in consensus. General visualization of the LA was rated on the following five-point scale: (1) excellent depiction with smooth endocardial surface; (2) good depiction with only discrete irregularities of the endocardial surface; (3) moderate depiction with moderate irregularities of the endocardial surface; (4) poor depiction with severe irregularities of the endocardial surface; and (5) segmentation of LA failed. One blinded reader (T.V.) processed the fusion of the EAM data with the CT image. The registration error between the surface of segmented LA and the mapping points of three-dimensional EAM was calculated automatically by the software of the EAM system. The accuracy of LA reconstructions was expressed as the mean distance between the EAM points and the surface of the segmented LA.
Calculation of patient radiation exposure
The dose–length product (DLP) was calculated by the scanner for each patient. Dedicated software (CT-Expo V1.6 2007, Medical University Hannover, Germany) was used for the calculation of effective doses. 20
Statistical analysis
Mean value and standard deviation were calculated for quantitative data. Normal distribution of the quantitative data was verified using the Kolmogorov–Smirnov test. A two-tailed unpaired Student's t -test was then used to evaluate the significance of differences between groups with regard to segmentation procedure time, radiation exposure, and registration error. The χ 2 test was used to test for significant differences of qualitative image scores between LA reconstructions from non-gated and ECG-gated MDCT. Statistical significance was assumed at a P -value <0.05.
Results
Computed tomographic imaging and LA segmentation were successfully completed in all patients. Non-gated MDCT was performed with a mean DLP of 230 ± 58 mGy * cm and a mean effective dose of 4.6 ± 1.4 mSv. Mean DLP and mean effective dose of ECG-gated MDCT were 667 ± 171 mGy * cm and 13.4 ± 3.6 mSv, respectively. Hence, ECG-gated MDCT exposed the patients to a significantly higher radiation dose ( P < 0.001).
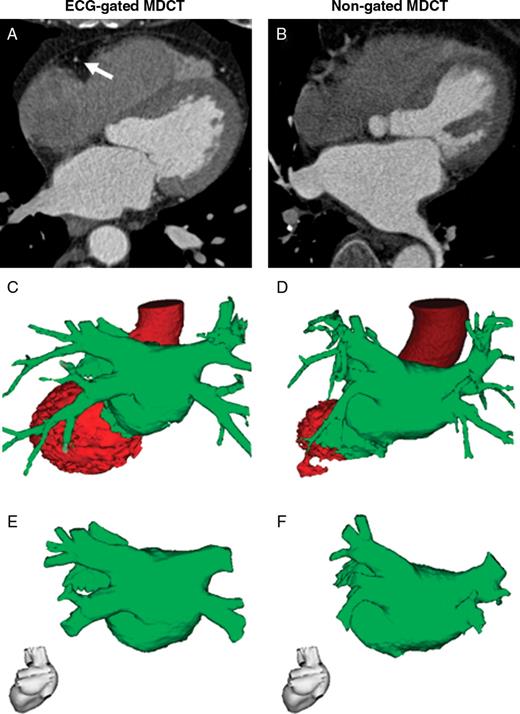
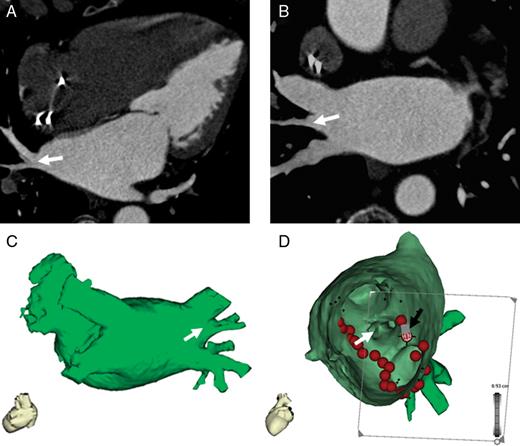
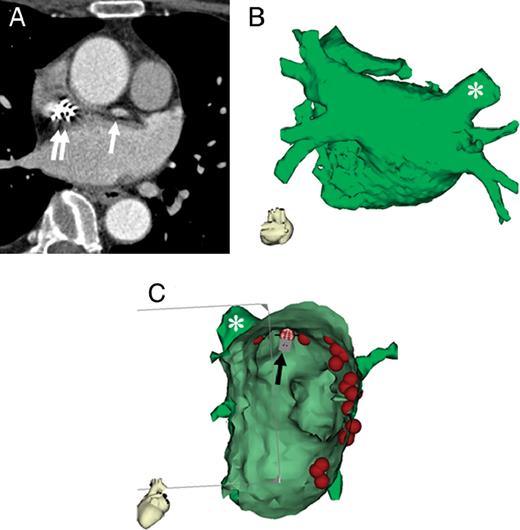
Segmentation of LA from MDCT data took 2:31 ± 0:54 min for non-gated MDCT and 2:36 ± 0:47 min for ECG-gated MDCT ( P = 0.8). Representative LA segmentations from non-gated and ECG-gated MDCT data sets are shown in Figure 1 . Non-gated MDCT allowed for LA segmentation with excellent or good image quality in 14 out of 15 patients ( Table 1 and Figure 2 ). In one patient, image quality of LA reconstruction of non-gated MDCT data was rated as moderate due to motion artefacts and streak artefacts from pacemaker leads ( Figure 3 ). Mean image quality scores of LA reconstruction from non-gated and ECG-gated MDCT were 1.3 ± 0.6 and 1.4 ± 0.7, respectively, with no statistical difference between non-gated and ECG-gated MDCT ( Table 1 , P = 0.76).
Image quality of reconstructions of the LA from ECG-gated and non-gated MDCT
| . | ECG-gated MDCT . | Non-gated MDCT . |
|---|---|---|
| Excellent (1) | 10 | 11 |
| Good (2) | 2 | 3 |
| Moderate (3) | 2 | 1 |
| Poor (4) | 0 | 0 |
| Failed (5) | 0 | 0 |
| Mean ± SD | 1.4 ± 0.7 | 1.3 ± 0.6 |
| . | ECG-gated MDCT . | Non-gated MDCT . |
|---|---|---|
| Excellent (1) | 10 | 11 |
| Good (2) | 2 | 3 |
| Moderate (3) | 2 | 1 |
| Poor (4) | 0 | 0 |
| Failed (5) | 0 | 0 |
| Mean ± SD | 1.4 ± 0.7 | 1.3 ± 0.6 |
ECG, electrocardiogram; MDCT, multi-detector-row computed tomography; SD, standard deviation.
Image quality of reconstructions of the LA from ECG-gated and non-gated MDCT
| . | ECG-gated MDCT . | Non-gated MDCT . |
|---|---|---|
| Excellent (1) | 10 | 11 |
| Good (2) | 2 | 3 |
| Moderate (3) | 2 | 1 |
| Poor (4) | 0 | 0 |
| Failed (5) | 0 | 0 |
| Mean ± SD | 1.4 ± 0.7 | 1.3 ± 0.6 |
| . | ECG-gated MDCT . | Non-gated MDCT . |
|---|---|---|
| Excellent (1) | 10 | 11 |
| Good (2) | 2 | 3 |
| Moderate (3) | 2 | 1 |
| Poor (4) | 0 | 0 |
| Failed (5) | 0 | 0 |
| Mean ± SD | 1.4 ± 0.7 | 1.3 ± 0.6 |
ECG, electrocardiogram; MDCT, multi-detector-row computed tomography; SD, standard deviation.
Segmentation of LA from MDCT data sets. Segmentation of ECG-gated ( A , C , and E ) and non-gated ( B , D , and F ) MDCT data sets was performed using the CartoMerge™ Image Integration Module. Shown are representative axial images of MDCT data sets ( A and B ), the corresponding semi-automatic segmentation results ( C and D ), and the final reconstruction of the LA after manual editing ( E and F ). Note that ECG-gated MDCT ( A ) clearly depicted the right coronary artery (marked with an arrow), whereas the right coronary artery was severely blurred on non-gated MDCT due to motion artefacts ( B ).
Reconstruction of the LA from non-gated MDCT with excellent image quality. Pulmonary vein isolation was performed using LA reconstruction from non-gated MDCT (75-year-old woman with paroxysmal AF and implanted pacemaker). Shown are a representative axial image ( A ), paraaxial image ( B ), corresponding LA reconstruction ( C ), and the fused electroanatomic map ( D , view from inside of the LA to right PVs). The right middle PV (white arrow) is clearly visualized. Tags on fused electroanatomic map indicate sites of radiofrequency current delivery. The black arrow indicates the position of the ablation catheter performing an ablation at the posterior part of the ridge between the right inferior PV and the middle PV.
Reconstruction of the LA from non-gated MDCT with moderate image quality. A 59-year-old woman with moderate image quality of non-gated MDCT ( A ) due to motion artefacts from pronounced atrial contraction (white arrow) and streak artefacts from pacemaker leads (white double arrow). Despite moderate irregularities of the endocardial surface, LA reconstruction ( B ) had sufficient image quality for integrated EAM ( C , view from inside of the LA to right PVs). Tags on fused electroanatomic map indicate sites of radiofrequency current delivery. The black arrow indicates the position of the ablation catheter performing ablation at the superior part of the ostium of right superior PV (marked with asterisk).
In all patients, LA reconstruction from MDCT was successfully aligned with LA geometry obtained from EAM. The mean number of map points collected from EAM was 92 ± 31 (range 58–168). The mean distance between EAM map points and the LA reconstructions of non-gated and ECG-gated MDCT data was 1.8 ± 0.2 mm (range 1.2–2.1 mm) and 1.9 ± 0.3 mm (range 1.5–2.4 mm), respectively ( P = 0.6).
Discussion
Reduction of radiation exposure is a critical issue in patients undergoing PVI, since these patients receive a significant radiation dose from procedural fluoroscopy, especially when complex ablation techniques are performed. Moreover, these patients are often scheduled for follow-up examinations and re-interventions. To the best of our knowledge, the current study is the first to evaluate the use of non-gated 64-detector-row CT for imaging of LA in comparison to ECG-gated 64-detector-row CT. Our data indicate that non-gated MDCT depicts LA with adequate image quality and significantly reduced radiation exposure compared with ECG-gated MDCT.
Atrial fibrillation is the most common sustained cardiac arrhythmia. 21 Atrial fibrillation episodes are frequently triggered by ectopic beats that arise within or near the origin of the PVs. 1 , 22 Electrophysiology studies have suggested that the combination of abnormal automaticity, induced triggered activity, and multiple re-entrant circuits is the underlying mechanism of arrhythmogenic activity of the PVs. 23 In many cases, myocardial sleeves that extent from the LA into the PVs are considered as the source of arrhythmogenic activity associated with AF initiation and maintenance. 24–29 Electrical PVI through catheter-based delivery of radiofrequency energy blocks conduction of ectopic beats from the PVs and prevents initiation of AF. 2 In many centres, PVI is performed using EAM systems, which allow for non-fluoroscopic catheter navigation. 30 Computed tomographic images of the LA are commonly integrated into these EAM systems to improve anatomic orientation and catheter navigation.
Current MDCT protocols for LA imaging prior to PVI recommend CT scanners with at least 16 detector rows and fast gantry rotation speed to minimize artefacts due to cardiac motion. 6 In spiral MDCT, radiation dose is inversely proportional to pitch. 31 Pitch refers to the ratio of table increment (the distance the table is advanced per rotation of the X-ray tube) to total nominal beam width (sum of all individual detector widths). Retrospectively ECG-gated MDCT is usually performed with low pitch values for high data oversampling which allows image reconstructions at any time point within the cardiac cycle—so-called isophasic image reconstruction. The disadvantage of low pitch scanning, however, is the increased radiation dose due to acquisition of highly overlapping slices. In contrast, non-gated MDCT uses high pitch values and therefore expose the patient to substantially lower radiation dose. The trade-off of using high pitch is that the images cannot be reconstructed at different time points within the cardiac cycle (i.e. no isophasic image reconstruction), making this technique more susceptible to motion artefacts. Motion artefacts with non-gated MDCT preclude its use for evaluation of the coronary arteries, but are acceptable for larger and less mobile cardiac structures such as the LA.
Most of the studies of LA imaging used CT protocols with retrospective ECG-gating and low pitch values as applied also for coronary CT angiography. 5 , 9 , 11–14 , 19 , 32 , 33 In our study, ECG-gated MDCT exposed the patients to a mean radiation dose of 13.4 ± 3.6 mSv. The radiation dose is hereby in good accordance with recently published studies on coronary CT angiography using 64-detector-row CT scanners with a slice collimation of at least 0.6 mm, which reported patient radiation exposure of ∼15 mSv. 18 , 34 The somewhat lower radiation exposure in our study could be explained by the fact that PV imaging requires shorter z -axis coverage compared with coronary CT angiography. Only few studies on CT imaging prior to PVI mention the effective radiation dose associated with MDCT. Cronin et al . 35 used ECG-gated MDCT for measurements of PV geometry in patients referred to PVI. In their study, ECG-gated CT imaging on a 16-detector-row CT scanner using a collimated slice thickness of 1.25 mm exposed the patients to a radiation dose of ∼10 mSv. Weber et al . 17 performed ECG-gated CT imaging of the LA using an increased collimated slice thickness of 1.5 mm in an effort to reduce radiation exposure, which resulted in an effective radiation dose of 8.5 ± 0.3 mSv. In addition, Weber et al . evaluated the impact of pre-interventional CT imaging on fluoroscopy time and radiation dose from procedural fluoroscopy. Integration of CT data sets into the ablation procedure reduced fluoroscopy time by a mean of 9 min. However, the additive radiation dose of cardiac CT was too high to provide a significant reduction of the overall patient radiation exposure. Weber et al . therefore concluded that there is still a need for optimized low radiation dose CT protocols for LA imaging.
In the present study, we evaluated the use of non-gated MDCT for imaging of the LA prior to PVI. We performed CT imaging on a 64-detector-row CT scanner with a collimation of 0.6 mm and a reconstructed slice thickness of 0.75 mm. The mean radiation dose of non-gated MDCT was 4.6 ± 1.4 mSv. Hence, our 64-detector-row CT protocol exposed the patients to a significantly lower radiation dose than the ‘low dose’ CT protocol proposed by Weber et al . while providing improved spatial resolution. 17 Qualitative evaluation of image quality of non-gated and ECG-gated MDCT demonstrated reliable visualization of the LA with both imaging approaches. In addition to qualitative evaluation, we also performed quantitative assessment of the accuracy of MDCT as proposed by Martinek et al . 19 Fusion of LA reconstructions of non-gated MDCT with EAM indicated a mean registration error of 1.8 ± 0.2 mm. Our data are therefore in good accordance with the study of Martinek et al ., who reported a mean registration error of 1.6 ± 1.2 mm for their ECG-gated 16-detector-row CT protocol. More importantly, there was no significant difference in matching accuracy between non-gated and ECG-gated MDCT in our patient collective.
Frequently cited advantages of ECG-gating include the ability to know in which part of the cardiac cycle the PV diameters were measured. Indeed, PV ostial diameter can vary by 11–23% between atrial systole and atrial diastole. 36 Error in PV diameter measurements could be problematic in choosing appropriately sized circular or balloon-based ablation catheters, as well as in evaluation of post-procedural PV stenosis. It should be noted, however, that changes in patient volume status between imaging and PVI procedure can also cause significant variation in PV diameter. 6 Furthermore, recommendations for intervention in post-procedural PV stenosis are reserved for symptomatic patients with severe stenosis (>70% lumen diameter reduction), who are unlikely to be misdiagnosed on the basis of phasic changes in PV diameter. Non-gated MDCT therefore provides sufficient image quality to rule out significant PV stenosis. 8
Since the introduction of MDCT, there has been a trend in shortening scanning time and reducing radiation dose by increasing the width of detector coverage. 37 The introduction of 64-detector-row CT scanners greatly improved the image quality of retrospective ECG-gated cardiac imaging in comparison to former CT scanners. Furthermore, 64-detector-row CT provided the opportunity for prospective ECG-gated cardiac imaging in reasonable scan times with a consecutive reduction of patient radiation exposure to 2.1 mSv. 38 Prospective ECG-gated cardiac imaging using 64-detector-row CT scanners, however, suffered from limitations including motion artefacts and stair-step artefacts caused by incorrect fusion of two adjacent data sets. 38 These drawbacks could be overcome by single-beat cardiac CT imaging using the recently introduced dual-source CT or wide-area detector CT. 39 , 40 However, access to both these new scanner systems is still relatively limited.
Some limitations of our study deserve mention. Major limitations of the study are the retrospective design and the limited number of patients. Our study unintentionally included a higher proportion of women compared with larger studies of PVI. 41 , 42 Our gender distribution is most likely attributable to our small sample size and regional variations in patient demographics referred for PVI. Women remain an important group of patients referred for PVI and in fact may receive more benefit than men from low radiation MDCT protocols because of their radiation-sensitive breast tissue. Ultimately, we do not feel that our patient demographics significantly influence our conclusions regarding the evaluation of MDCT protocols prior to PVI. Another limitation of the study is the fact that we included only patients who were in sinus rhythm during both CT imaging and PVI. Hence, final appraisal of the most effective MDCT protocol is possible only in a larger prospective study comparing ECG-gated and non-gated MDCT, including patients with cardiac arrhythmias. However, we believe that the inclusion of patients with cardiac arrhythmias would not substantially change the main finding of our study that non-gated MDCT depicts the LA with image quality comparable to ECG-gated MDCT. This is due to the fact that the latter is even more susceptible to heart rhythm irregularities. Moreover, former studies indicated that cardiac rhythm does not influence the accuracy of LA reconstructions from MDCT data. 19 , 33
In conclusion, non-gated MDCT of LA and PVs yields comparable image quality to ECG-gated MDCT. However, non-gated MDCT was acquired with a significantly reduced patient radiation exposure. Our data suggest that pre-procedural imaging with non-gated MDCT is a reasonable alternative to ECG-gated MDCT, yet comparability of clinical outcomes requires demonstration in further studies.
Conflict of interest: A.H. has been a full-time, paid employee of Siemens AG since 1 June 2004 and his function is Associate Director of the Imaging Science Institute Charité Berlin. The Institute is a scientific cooperation between the Charité, University Hospitals of Berlin and Siemens Healthcare in the form of a private–public partnership. T.V. receives speaker's honoraria from Biosense Webster.